A Practical Approach to Teaching Systems-Based Practice
Lisa Weiss, MD, MEd; Susan Labuda-Schrop, PhD; LuAnne Stockton, BS, BA
Systems-based practice is defined by the Accreditation Council for Graduate Medical Education (ACGME) as actions that demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to call on system resources effectively to provide care that is of optimal value. Medical students are now asked to have this knowledge before they get to residency. With the emphasis on interprofessional education and teamwork, systems-based practice has become a “hot” topic. Systems-based practice is one of the most challenging competencies to define, incorporate into training and practice, and evaluate.1 Clerkship educators have struggled with ways in which to incorporate concepts related to systems-based practice into the curriculum as well as how to evaluate students’ achievement of understanding and application of the concept.
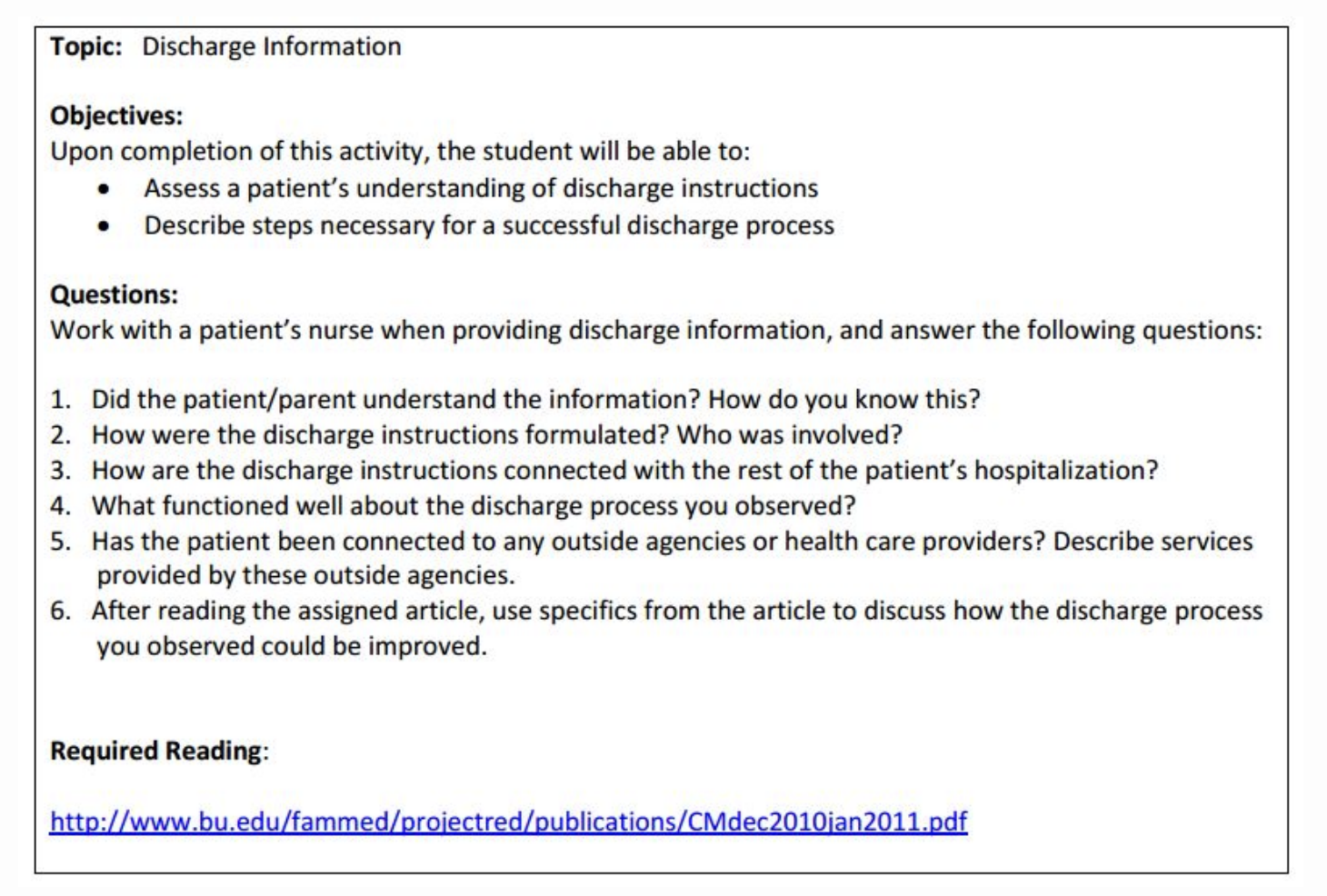
To incorporate systems-based practice concepts into undergraduate medical education, we embedded a systems-based practice curriculum into third-year clerkships without significantly adding to the faculty or student workload or disrupting the clerkship rotation. Our Health Systems Questions curriculum is one part of a longitudinal course in the third year. Students are assigned sets of questions on topics such as team-based care, patient safety, hospital readmissions, use of evidence-based medicine, transitions of care, and care for the underserved, including social determinants of health. They access and respond to questions using an asynchronous online instructional approach. Questions focused on one of the topics, including resources for students to refer to in responding to the questions, are assigned during each clerkship rotation. Students respond to the questions online in written format. Questions and references are designed so that the process encourages students to give critical consideration to the clinical and administrative world occurring around them. To complete the circle, students receive feedback from volunteer faculty who include senior residents, primary care physicians, specialty physicians, and, in coming months, doctoral nursing students. These faculty electronically respond to the students’ answers in relation to the resources as well as share personal stories of similar situations that encourage students to think more deeply about the topic at hand. We offer the following example of a question set:

Organizing the embedded questions with 140 students and numerous volunteer faculty all online has been challenging. Recruiting and training enough faculty to evaluate the student responses, determining what level of response is appropriate, and follow-up for “problematic” students such as those who have inadequate or late responses takes administrative finesse.
Overall, however, this experience is well received by students who report that the questions are applicable to experiences they encounter during their clerkship rotations. Through annual program evaluation and anecdotal comments, faculty indicate that the curriculum encourages students to think about and respond to these situations. The curriculum also provides educators with a means to evaluate students formally in this competency. The Health Systems Questions curriculum provides a unique, effective way to involve the students in learning about and applying the concept of systems-based care.
Reference
1. Johnson JK, Miller SH, Horowitz SD. Systems-based practice: improving the safety and quality of patient care by recognizing and improving the systems in which we work. In: Henriksen K, Battles JB, Keyes MA, et al, eds. Advances in patient safety: new directions and alternative approaches (Vol. 2: Culture and redesign). Rockville, MD: Agency for Healthcare Research and Quality, Aug 2008.