“Save Time, Reduce Burnout”: The Creation of a Novel Curriculum on EHR In-basket Management at a Family Medicine Residency
by Shaylagh Cerulli, MD, Cambridge Health Alliance, Cambridge, MA; Roberta Dennison, MD, Cambridge Health Alliance, Cambridge, MA; Jessica Early, MD, Cambridge Health Alliance, Cambridge, MA; Ashley King, MD, MPH, MS, Kaiser Permanente Mid-Atlantic, Rockville, MD; Joy Lee, MD, MPP, Kaiser Permanente Mid-Atlantic, Rockville, MD; Deidre Patel, MD, Newton Wellesley Hospital, Newton, MA; Omar Wahid, MD, Cambridge Health Alliance, Cambridge, MA
Background
Primary care's scope includes managing patient concerns after they have left the clinic. A primary care clinician’s ability to manage electronic health record (EHR)-generated in-basket work influences overall job satisfaction and rates of burnout.1,3,4-6 Motivated by resident feedback, our project-based improvement team of residents and faculty sought to create a formal curriculum on in-basket management for our EHR. Our team completed a needs assessment encompassing current in-basket management curricular activities to increase resident satisfaction and confidence while reducing burnout. We hoped to build on the residency EHR training research to provide a guide for other programs.2
Intervention
Our team completed a needs assessment encompassing current in-basket management. This needs assessment included a literature review, a survey of local family medicine residency programs, a review of recommendations from professional bodies within family medicine, and a survey of our own faculty and residents. We also attended EPIC and in-basket efficiency sessions to better understand what resources were available.
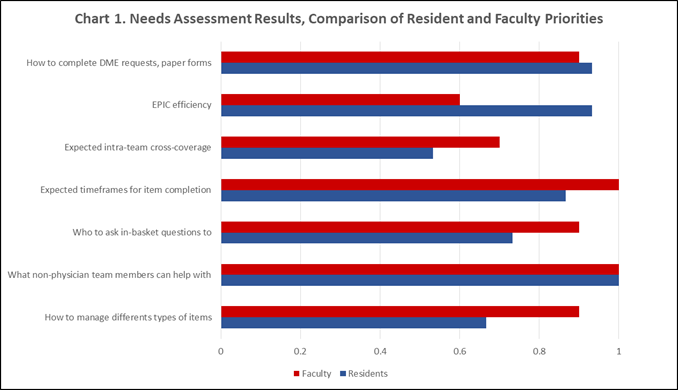
Our literature search found that the majority of published data relate to the pitfalls of EHR-generated work without recommending how to manage this work.1,3,5-6 For our internal survey, residents, and faculty were asked which areas of EHR management they felt they needed more education on. Overall, both faculty and residents felt that more education was needed on almost all identified topics (Figure 1). Our survey highlighted the absence of clearly articulated expectations and our residents’ desire for more structured efficiency tips, as well as timely mentorship. EHR in-basket topics included paper forms, efficiency, cross-coverage, time frames for completion, resident supervision, and use of health care team members.
Figure 1: Needs Assessment Results, Comparison of Resident and Faculty Priorities
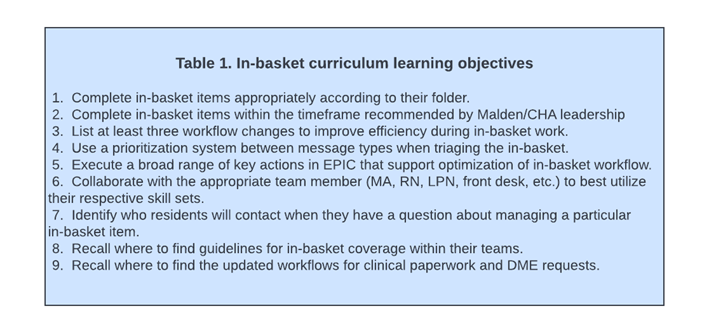
Based on the results of our needs assessment, we identified learning objectives for our new curriculum and created a curriculum matrix to guide the teaching and assessment of these topics to achieve our objectives. Table 1 shows our final learning objectives.
Table 1: In-basket Curriculum Learning Objectives
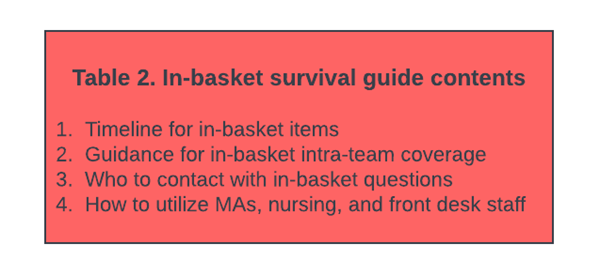
Our new curriculum includes many components, including several didactic sessions, recommendations for preceptors, and clear guidelines on in-basket management topics including turnaround time, use of health care team members, and resident precepting workflows. The most well-received implementation from our curricula was creating and distributing an “in-basket survival guide” to be added to our residency survival guide and handbook. The main content areas included in this survival guide are shown in Table 2.
Table 2: In-Basket Survival Guide Content
Conclusions and Recommendations
The structure of team in-basket management and curriculum development used here can be extrapolated to other residencies to improve both the quality of learning and care involved in asynchronous patient care. Specifically, the content areas included in our in-basket survival guide can be extrapolated to other programs by identifying the guidelines for these topics within the health care institution and focusing on these topics for resident education.
Next directions for this project include studying whether our interventions improved resident skills and knowledge of in-basket management and reduced burnout.
References
- Akbar F, Mark G, Warton EM, et al. Physicians’ electronic inbox work patterns and factors associated with high inbox work duration. J Am Med Inform Assoc. 2021;28(5):923-930. doi:10.1093/jamia/ocaa229
- Kim JG, Rodriguez HP, Estlin KA, Morris CG. Impact of Longitudinal Electronic Health Record Training for Residents Preparing for Practice in Patient-Centered Medical Homes. Perm J. 2017;21(3):16-122. doi:10.7812/TPP/16-122
- Lieu TA, Altschuler A, Weiner JZ, et al. Primary Care Physicians’ Experiences With and Strategies for Managing Electronic Messages. JAMA Netw Open. 2019;2(12):e1918287. doi:10.1001/jamanetworkopen.2019.18287
- Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine (Baltimore). 2018;97(38):e12319. doi:10.1097/MD.0000000000012319
- Sinsky C, Colligan L, Li L, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165(11):753-760. doi:10.7326/M16-0961
- ran B, Lenhart A, Ross R, Dorr DA. Burnout and EHR use among academic primary care physicians with varied clinical workloads. AMIA Jt Summits Transl Sci Proc. 2019;2019:136-144. Published 2019 May 6.
