Implementation of Residents as Teachers Curriculum in a New Family Medicine Residency Program
by Sumira Koirala, MD and Lisa Weiss, MD, St. Elizabeth Boardman Family Medicine Residency, Boardman, OH.
Background
The Accreditation Council for Graduate Medical Education (ACGME) recognizes the important role of residents as teachers and recommends that senior residents serve in supervisory roles during their training. This recognizes their progress toward independence.4,7 The Liaison Committee on Medical Education (LCME) also emphasizes the need for structured programs to enhance residents’ teaching skills.5,6 In addition to teaching medical students, residents supervise their junior peers and educate patients. Many residency programs are now adopting residents-as-teachers (RaT) curricula to formally train residents to teach. In a new residency program, our residents had limited to no exposure to senior residents as teachers; as such, we implemented a RaT curriculum to formally train our residents with the necessary skills to become effective teachers and to improve the education of our residents and students in their development as clinicians.
Implementation
A 2.5-hour workshop on teaching skills and giving feedback was presented to our second- and third-year residents in July 2019 and 2020. We used the STFM Faculty for Tomorrow RaT curriculum. The session was interactive and included role playing. The main objectives of the first half of the session were to define teaching versus learning, explain the basic tenets of adult learning theory, examine how learning generally develops among students and residents, and describe specific types of case-based teaching techniques like Priming, Framing, Modelling, and the use of the One-Minute Preceptor.
The second half of the session focused on learning how to give effective feedback. The objectives for this part of the session were to define feedback, discuss the importance of giving and receiving feedback, describe the characteristics of effective feedback, describe strategies for delivering feedback (the feedback sandwich, modified feedback sandwich, and the ARCH Model), and apply feedback strategies to scenarios.
Methods for Measuring Outcomes
The second- and third-year residents who received the training in 2019 were surveyed using an anonymous paper survey with open-ended questions 5 months after the session to test retention of the RaT material. The residents were asked which techniques they were using. In 2020, we implemented a pre- and postintervention survey using an anonymous paper survey. We used Likert scales on this survey to assess the knowledge about teaching, confidence in teaching, and change in approach to teach after attending the session. The participation rate was 100% in both years. The first-year residents who did not participate in the workshop were also surveyed anonymously on paper asking about their interest to participate in the future. Additionally, the students who rotated through our family medicine residency program between November 2019 to March 2020 were surveyed anonymously on paper using open-ended questions regarding the teaching and feedback they received from our residents.
Results
The 2019 data indicated that they mostly used the priming, framing, and one-minute precepting principles and feedback sandwich approach. The residents reported that the workshop reinforced their approach and knowledge of teaching the junior interns and medical students and increased their confidence in teaching.
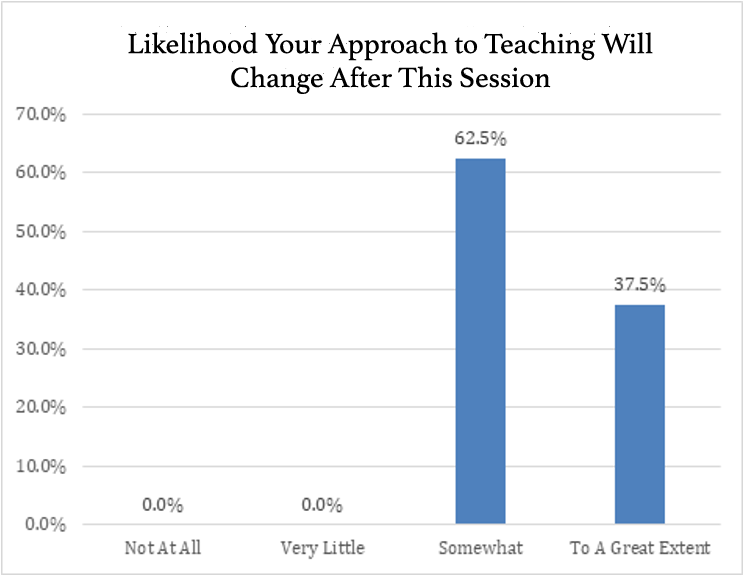
The results of the 2020 survey are shown in Figures 1-3. Participants who responded “somewhat” in Figure 3 reported that they will start to use priming and framing more often. The participants who responded “to a great extent” reported that they will start using priming and framing along with one-minute principles and will give feedback using the modified feedback sandwich.
Figure 1: Knowledge About Teaching Junior Residents and Medical Students
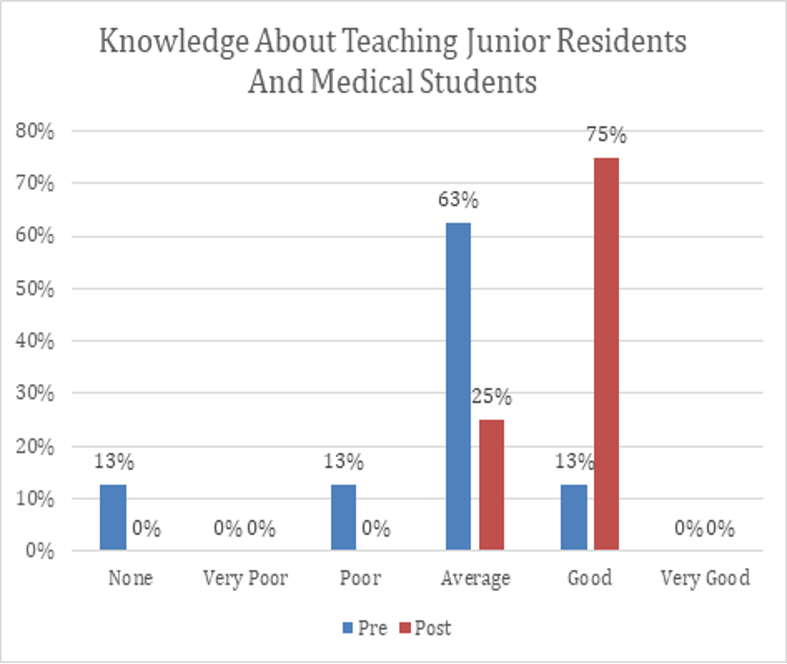
Figure 2: Confidence in Teaching
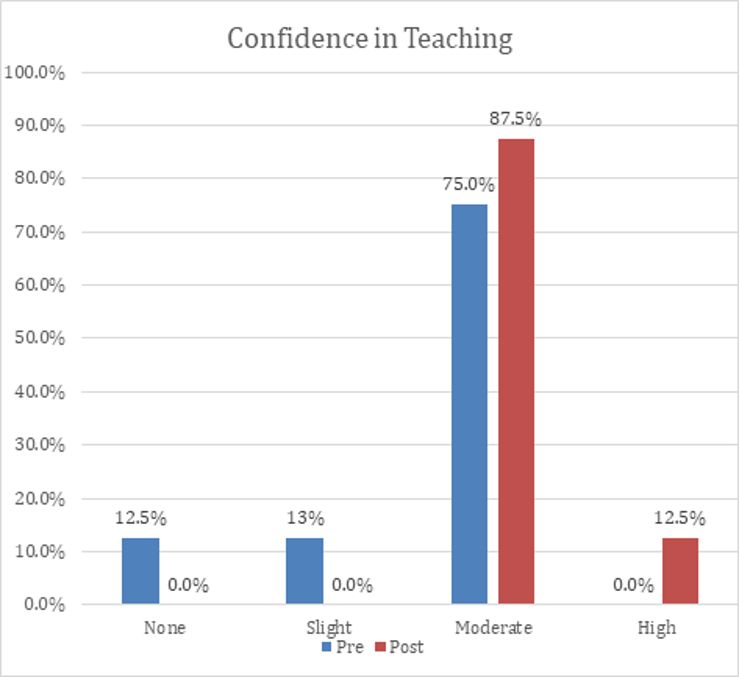
Figure 3: Likelihood Your Approach to Teaching Will Change After This Session
First-year residents demonstrated willingness to participate in a formal workshop to enhance their teaching skills. One hundred percent of rotating students reported that they found the residents’ teaching to be effective and that they received feedback regularly.
Conclusion
Studies estimate that residents spend up to 20% of their time on teaching.1 Residents enjoy teaching and consider it important for their own education.2 Studies have also found that residents assigned to teaching activities increased their knowledge acquisition of the assigned topics.3 Residents, who are good teachers, seem to have a good content of medical knowledge and clinical skills.8 Medical students attribute one-third of their clinical education to teaching from interns and residents.10 Our results indicate that even a limited amount of formal instruction in teaching can reinforce the residents’ approach and knowledge of teaching and improve their confidence and the way students evaluate them. Our residents have indicated that they want more frequent feedback on their teaching, and we are in the process of implementing this in upcoming years. Implementation of the RaT curriculum can be beneficial for all residency programs.
References
- Greenberg LW, Goldberg RM, Jewett LS. Teaching in the clinical setting: factors influencing residents’ perceptions, confidence and behaviour. Med Educ. 1984;18(5):360-365. doi:10.1111/j.1365-2923.1984.tb01283.x
- Apter A, Metzger R, Glassroth J. Residents’ perceptions of their role as teachers. J Med Educ. 1988;63(12):900-905.
- Tremonti LP, Biddle WB. Teaching behaviors of residents and faculty members. J Med Educ. 1982;57(11):854-859. doi:10.1097/00001888-198211000-00006
- Bree KK, Whicker SA, Fromme HB, Paik S, Greenberg L. Residents-as-teachers publications: what can programs learn from the literature when starting a new or refining an established curriculum? J Grad Med Educ. 2014;6(2):237-248. doi:10.4300/JGME-D-13-00308.1
- Karani R, Fromme HB, Cayea D, Muller D, Schwartz A, Harris IB. How medical students learn from residents in the workplace: a qualitative study. Acad Med. 2014;89(3):490-496. doi:10.1097/ACM.0000000000000141
- Liaison Committee on Medical Education Functions and Structure of a Medical School. [Accessed December 19, 2014]. Available from: https://med.virginia.edu/ume-curriculum/wp-content/uploads/sites/216/2016/07/2017-18_Functions-and-Structure_2016-03-24.pdf.
- The family medicine milestone project. J Grad Med Educ. 2014;6(1 Suppl 1):74-86. doi:10.4300/JGME-06-01s1-05. Accessed December 19, 2014.
- Falcone JL, Ferson PF, Hamad GG. S/he who can, does and teaches. S/he who cannot, doesn’t. J Surg Educ. 2014;71(1):96-10.1 doi:10.1016/j.jsurg.2013.06.003
- Morrison EH, Friedland JA, Boker J, Rucker L, Hollingshead J, Murata P. Residents-as-teachers training in U.S. residency programs and offices of graduate medical education. Acad Med. 2001;76(10)(suppl):S1-S4. PubMed. Google Scholar. doi:10.1097/00001888-200110001-00002
- Whitman N, Schwenk T. Residents As Teachers: A Guide to Educational Practice. 3rded. Pacific Grove, CA: Whittman Associates; 2005.
