A Multidisciplinary Approach to Quality Improvement: An Innovative Teaching Intervention for Medical Students
by Malvika Sharma, MD; Amythest Gauthier, MD; Amara Decker, MD, MPH; Allison Porter, MD; and John R McConaghy, MD; The Ohio State University Department of Family and Community Medicine
Background
Quality improvement (QI) is a process that comprises systematic actions that lead to enhancement of health care services and health conditions of target patient groups.1 An effective QI process involves partnership from multiple stakeholders in the health care setting.2 At the Ohio State University Rardin Family Practice, a multidisciplinary team consisting of medical students, family medicine residents, and medical assistants worked together to design a quality improvement project. Medical students were involved in the quality improvement process through the Applied Health Systems Science (AHSS) Program, a longitudinal course designed to train medical students on the basics of health systems, patient safety, quality improvement, informatics, and population health. The medical students received three structured lectures covering concepts such as root cause analysis, Five Whys methodology, cause and effect diagrams, the Lean Six Sigma method, and the methods of high-value care. The group identified that the blood pressure (BP) control rate (BP<140/90) in the clinic was was 57.1%, which is below the target of 70.94% set by Medicare’s Quality Program.
Intervention
The team created a protocol to implement self-monitored blood pressure control (SMBP) using Lean Six Sigma Methods. The protocol sought to raise patient awareness of the benefit of monitoring their blood pressure at home and educate them on how to record their blood pressure readings to discuss with their family physician. Patients were educated about SMBP using a poster mounted at eye level in the examination rooms. The poster was designed to invite conversation between patients and the medical assistants (MAs) about monitoring their blood pressure at home. The patients’ physician conducted the clinic visit with their patients as usual.
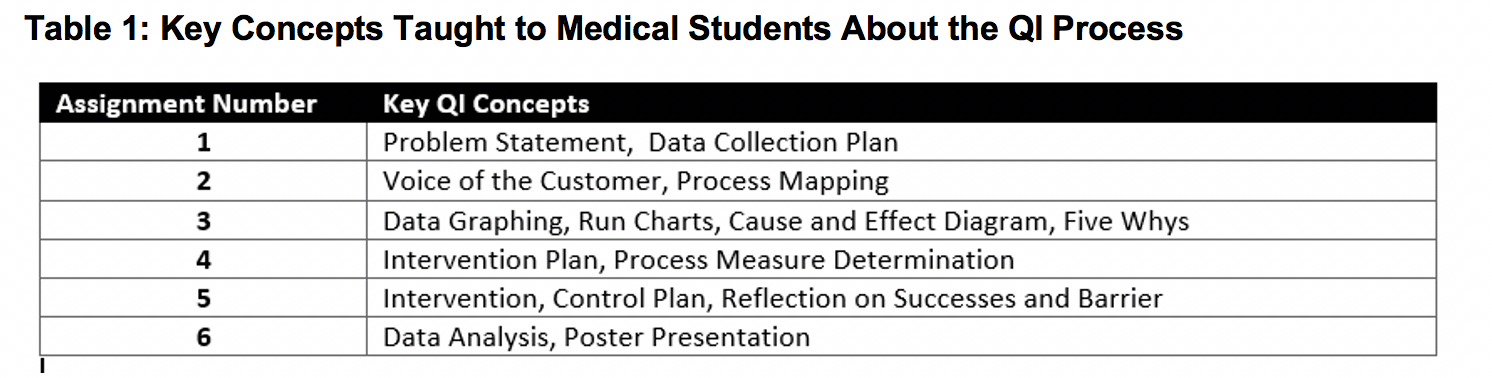
Medical students participating in the quality improvement process were evaluated through a written assignment due at each stage of the Lean Six Sigma method as shown in Table 1. The medical students collaborated with the family medicine residents for each assignment. The assignments were evaluated based on a rubric created to ensure comprehension of the QI process. The course culminated with a formal presentation given by the medical students and residents for the institution’s research symposium.
Results
At the culmination of the project the medical students and residents were given a postproject completion interview asking “What did you learn?” The medical students reported that they learned the process to define a problem, develop an intervention, implement the intervention, and develop the results. The residents reported that they learned that having a multidisciplinary team led to the intervention being applied at multiple levels of the system which led to quality improvement. This was also evident in the results of the intervention. The practice’s blood pressure control increased from 57.1% in September 2019 to 66% in February 2020. Both medical students and residents also learned the process of creating a poster and presenting the data through the culminating project.
Conclusions
This innovative teaching intervention educated medical students about the quality improvement process and gave them the opportunity to directly apply what they were learning. Medical students learned the concepts of quality improvement, needs assessment, implementation, and evaluation. Learning the Lean Six Sigma process resulted in improved team care which led to better blood pressure control in clinic. The medical students learned how to identify and make changes to improve the patient's experience of the health system. This multidisciplinary curriculum for quality improvement could be modeled at other institutions as well.
References
- US Department of Health and Human Services Health Resources and Services Administration. Quallity Improvement. Rockville, MD: HRSA; April, 2011. https://www.hrsa.gov/sites/default/files/quality/toolbox/508pdfs/qualityimprovement.pdf. Accessed May 21, 2021.
- Silver SA, Harel Z, McQuillan R, et al. How to begin a quality improvement project. Clin J Am Soc Nephrol. 2016;11(5):893-900. doi:10.2215/CJN.11491015
