A Novel, Interprofessional, Clinical Learning Experience for Family Medicine Residents
by Kelsie Kelly, MD, MPH; Ashley Crowl, PharmD; Laurel B. Witt, MD, Mphil; Hannah Maxfield, MD, Department of Family Medicine and Community Health, University of Kansas School of Medicine, Kansas City, KS
Background
Interprofessional (IP) leadership and collaboration are named among essential skills for graduate medical training in primary care. The Accreditation Council for Graduate Medical Education (ACGME) now mandates the inclusion of IP clinical opportunities, and Family Medicine (FM) Milestones 2.0 contains subcompetency ICS2, Interprofessional and Team Communication.1 Additionally, the National Academy of Sciences has defined high-quality primary care as interprofessional.2 Residency training in primary care specialties must involve opportunities to practice IP skills in both the inpatient and ambulatory settings.3 We found published examples of case-based didactic curricula covering IP concepts for residents.4-65 Few publications, however, exist that describe ambulatory practice models for training residents in IP skills during real patient care. Our aim was to study the effect of embedding FM residents in an established, clinic-based, IP learning and the practice environment.
Intervention
The IP Teaching Clinic (IPTC) has operated for more than a decade, set in the outpatient FM Clinic at the University of Kansas Medical Center, for the purpose of teaching IP skills to medical and health professions students. In the IPTC, IP student teams care collaboratively for real FM patients under the supervision of their faculty. Participating programs have included the schools/programs of medicine, pharmacy, nursing, psychology, and others. Students and faculty start each clinic session with IP team huddles. Student teams then synchronously evaluate a patient, the team then rehuddles before presenting to their IP faculty, and the visit is completed when the medicine attending accompanies the student team to the patient’s room. A dedicated debriefing on IP concepts and skills ends each clinic session.
In July 2019, IPTC was remodeled to embed postgraduate year-3 (PGY3) FM residents. Program goals were to enhance the residents’ supervised practice with essential IP competencies including teaming, feedback, and clinical teaching. This new IPTC-with-residents model asked the resident to stand in as the supervisor from medicine, receive (along with IP faculty and with medicine faculty supervision) the IP presentation from students, and complete the visit by returning with the student team to the patient room. The residents participated in the end-of-session debrief, as well. Residents were scheduled longitudinally in the IPTC throughout the year and cared for their own continuity patient panel during these sessions.
Results
We surveyed graduated residents and IPTC faculty to assess residents’ acquisition of teaming, feedback, and clinical teaching skills in August 2020. Three ACGME subcompetencies (shown in Table 1) aligned best with the IP concepts and skills-informed questions asked in these surveys. A scale of 1 to 5 was used, mirroring ACGME assessment levels 1 (novice) to 5 (expert). Supporting narrative comments were also collected. Five of 10 (50%) eligible IP faculty, and seven of nine (77%) eligible residents completed surveys.
Table 1: Family Medicine Milestones 2.0 Aligned With Interprofessional Competencies

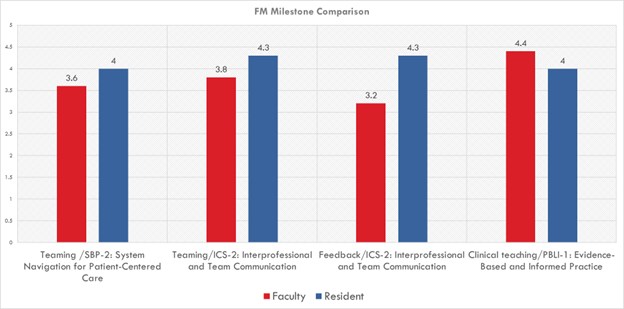
Residents and IP faculty rated the residents’ acquired IP skills highly overall. Interestingly, resident skills were evaluated more highly by the residents themselves (self-evaluation) than by the IP faculty in three of four competency areas (Figure 1).
Figure 1: ACGME Milestone-Rating Comparison Between Faculty and Residents
Residents were asked to provide narrative comments about their overall experience, and results were analyzed thematically. Themes included (1) residents valued the opportunity to teach, (2) they valued the opportunity to build comfort with IP skills and to practice leadership of teams, (3) they learned that IPTC seemed most beneficial for patients with medical complexity, and (4) the experience compelled them to reflect on how IP work might fit reasonably and sustainably into postresidency practice.
Conclusions
This innovation describes a model that allows residents to practice IP skills during real ambulatory patient care. As the model was well-received, preliminarily successful, and fulfills important IP residency training milestones, we have continued to use it at our training program. We believe the experience provided our residents with an opportunity to practice their leadership and collaboration skills in a way that may translate to future success in these roles after graduation, and future study would be useful to understand these effects. Other programs might implement similar training initiatives in a variety of ways, starting with relationship-building with nearby allied health professional schools.
References
- Family Medicine Milestones. Accreditation Council for Graduate Medical Education. Second Revision: October 2019. Accessed September 8, 2021. https://www.acgme.org/Portals/0/PDFs/Milestones/FamilyMedicineMilestones.pdf?ver=2020-09-01-150203-400
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Implementing High-Quality Primary Care, Robinson SK, Meisnere M, Phillips RL Jr., McCauley L, eds. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Washington, DC: National Academies Press; May 4, 2021.
- Arenson C, Brandt BF. The importance of interprofessional practice in family medicine residency education. Fam Med. 2021;53(7):548-555. doi:10.22454/FamMed.2021.151177
- Lounsbery JL, Moon J, Prasad S. Assessing collaboration between family medicine residents and pharmacy residents during an interprofessional paired visit. Fam Med. 2015;47(5):397-400.
- Nikiforova T, Spagnoletti CL, Rothenberger SD, Jeong K, Hasley PB. Implementation of case conferences to improve interprofessional collaboration in resident continuity clinic. South Med J. 2019;112(10):520-525. doi:10.14423/SMJ.0000000000001025
- Soones TN, O’Brien BC, Julian KA. Internal medicine residents’ perceptions of team-based care and its educational value in the continuity clinic: a qualitative study. J Gen Intern Med. 2015;30(9):1279-1285. doi:10.1007/s11606-015-3228-3
