Other Publications
Education Columns
Pediatric Obesity Care Redesign by Establishing Consistent Standardized Care Curriculum using Centering Concepts; A Successful Pilot
By Mahanoor Raza MD, WellSpan Good Samaritan Hospital Residency Program, Lebanon, Pennsylvania; Feroza Patel DO, WellSpan Good Samaritan Hospital Residency Program, Lebanon, Pennsylvania; Trajan Barrera DO, WellSpan Good Samaritan Hospital Residency Program, Lebanon, Pennsylvania; Erum Azhar, MD, MS, MHQS, CPPS, FACOG, Dignity Health East Valley Obstetrics & Gynecology Residency Program, Gilbert, AZ & Creighton University School of Medicine, Phoenix, AZ ; Sukhjeet Kamboj, MD, FAAFP, WellSpan Good Samaritan Hospital Residency Program, Lebanon, Pennsylvania; Abdul Waheed MD, MS PHS, CPE, FAAFP, Department of Family Medicine, Dignity Health Medical Group, Arizona & Creighton University School of Medicine, Phoenix, AZ
Background: Pediatric obesity is a significant public health issue linked to chronic diseases1 with a huge economic impact2. It disproportionately affects Hispanic/Latinx, Blacks, and other children from under-resourced communities and underprivileged backgrounds3. Our program currently serves around 1200 pediatric patients with obesity. The majority of these patients face socioeconomic adversity and belong to Latinx, Black, and/or other immigrant/refugee populations. Lebanon County lacks consistent and standardized care for pediatric obesity. Patient referrals to other health systems outside the county for specialized care result in lower "keepage" rates with potential revenue loss for the organization and an increase in the total cost of care. Additionally, inconsistent and inadequate care is provided because of social determinants of health including lack of transport, out-of-pocket expenses related to care network tiers, and loss in communication back to Primary Care Providers (PCPs). We developed a standardized Care Curriculum in response to this community need, addressing the lack of resources, awareness, and education for patients, residents, physicians, and AdvancedPractice Providers (APPs). There are many Obesity Curriculums that have been implemented, but very few that utilized centering concepts4.
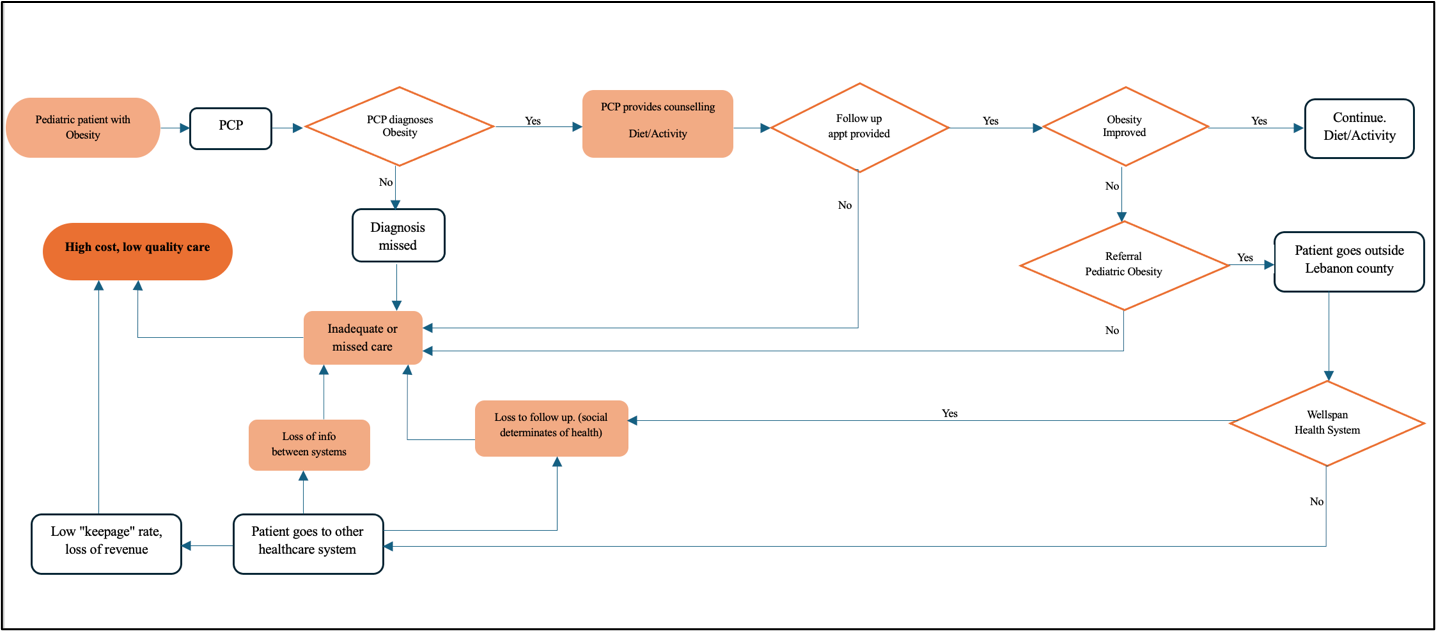
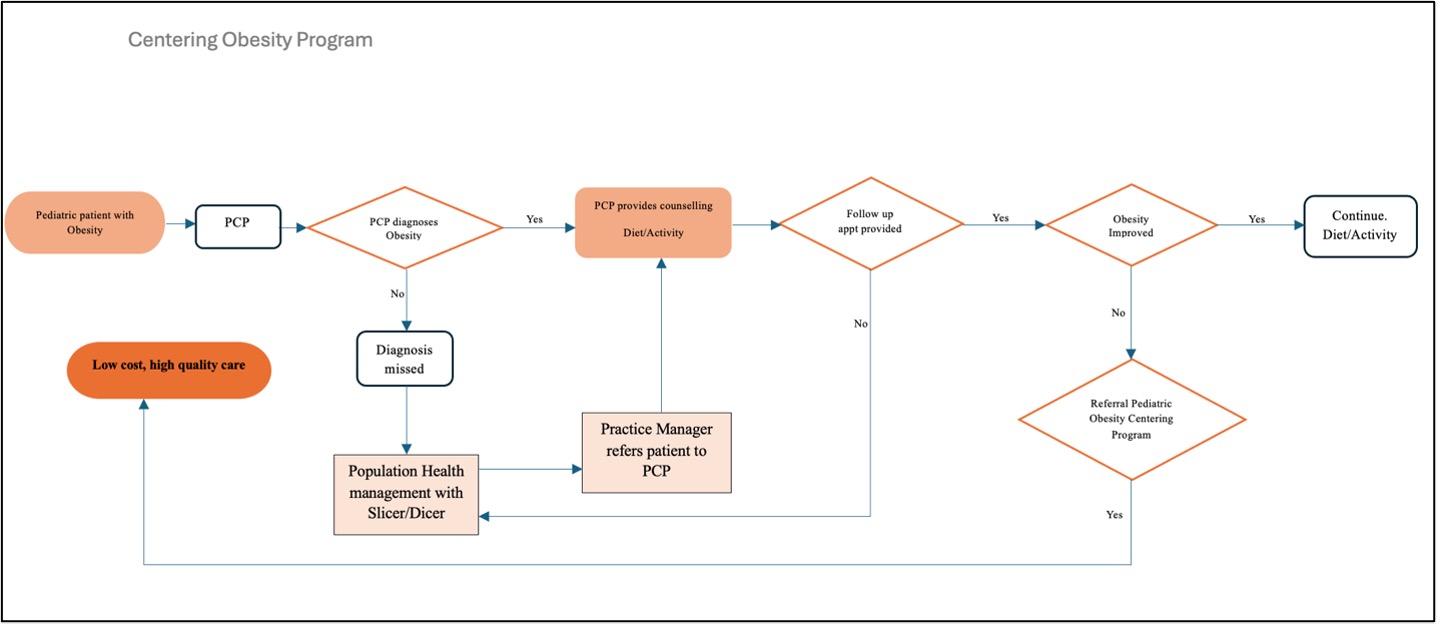
Implementation of the Intervention: This project utilized Lean methodology, a system which focuses on reduction of waste by fostering continuous feedback cycles, review, and learning, thus enhancing efficiency and becoming "lean." It helped redesign the care as a pilot project including setting up the charter and scope of the project, clear objectives, current process map, root cause analysis, future state, and progress timeline. Figure 1 and Figure 2 show the process map before and after root cause analysis and implementation of the bundled intervention to transform the care. This transformation required designing a Pediatric Obesity Centering Curriculum consisting of a 12-week intensive centering program for children 3-19 years with BMI > 95th percentile. The bundled intervention included:
- Curriculum for patients to learn the tenets of a healthy lifestyle highlighted in Table 1
- Curriculum for residents and faculty to learn the curriculum in A and ways to talk in common language
- Implementation of the care curriculum utilizing the redesigned process for standardized care
A group of six residents received training and participated in shared patient appointments and co-production using the centering concept.
Figure 1: Process map of current conditions of pediatric obesity care at Wellspan Good Samaritan Hospital family medicine residency program
Impact: A total of six kids with a BMI greater than the 95th percentile were enrolled in the program with their families. There were two males and four females in the group. The BMI ranged from 95.62 to 99.83 percentile at the baseline to 92.64 to 97.22 at the end of the program with a median weight loss of 0.69 percentile. A phone survey assessed retention factors and barriers, and positive feedback was received from the parents/guardians who attended the 12-week intensive centering program. The survey results and data on BMI change validated our post-intervention process map (Figure 2). Other studies have shown similar trends in BMI with incorporation of a standardized curriculum5. Resident focus group discussion also positively impacted their awareness, education, and a sense of giving back to the community through this curriculum. This was also portrayed amongst residents in another family medicine residency program with obesity education6.
Figure 2: Post-intervention Process map of the pediatric obesity care at Wellspan Good Samaritan Hospital family medicine residency program
Table 1: Table of Contents for Obesity Care Curriculum for Patients
|
Week 1 |
Introduction, Obesity as Health Condition, Health benefits of Weight loss/Knowing your Why (used for co-production of care delivery) |
|
Week 2 |
Review of last week, Overview of Healthy Diet, Physical Activity |
|
Week 3 |
Food diary, Calorie logging app, review motivation (used for co-production of care delivery) |
|
Week 4 |
Review of last week, Step Count, Cardio Exercise, Behavioral Challenges, Emotional management/Breakout Group discussion |
|
Week 5 |
Carbs vs protein vs fat, Portion sizes, Eating habits |
|
Week 6 |
Review of last week, Calisthenics on Youtube and other resources, Breakout Group discussion (used for co-production of care delivery) |
|
Week 7 |
How to read a label, Review portion sizes, Go over meal plan |
|
Week 8 |
Review of last week, Challenges and solutions/Breakout Group discussion (used for co-production of care delivery) |
|
Week 9 |
Hidden sugar, Healthy snacks, Walking efficiently, Exercise |
|
Week 10 |
Review of last week, Weight bearing exercises, Review of exercise resources on the web, indoor versus outdoor exercises, keeping track of physical activity |
|
Week 11 |
Rapid Review of Nutrition, Organic versus non-organic, Common Myth busting with diet and exercise, strategies for sustainable habits |
|
Week 12 |
Review Session/Summary, Possible medications/referrals, Small Group Breakout/Discussion (used for co-production of care delivery) |
Conclusion and Future Consideration: The overall evaluation of the pilot care redesign by the attendees was above average, and we achieved our aim to increase health literacy on healthy lifestyles, lower BMI, and identify system barriers for managing pediatric obesity. These findings will help scale the program for a larger population. Our specific aims for next academic year are:
- Determine Faculty FTE needed to maintain and grow these services to offer to patients cared for by the rest of WellSpan pediatrics/family medicine practices in Lebanon County
- Recruit and appoint faculty to supervise residents to continue to provide these services
- Offer a 200-hour Area of Concentration certificate with this curriculum to residents within WellSpan Health residency/fellowship programs
References:
- Balasundaram P, Krishna S. StatPearls [Internet] Treasure Island, Florida, USA: StatPearls Publishing; [ Jun; 2023 ]. 2023. Obesity effects on child health
- CDC. Health and economic costs of chronic diseases. Available at: https://www.cdc.gov/chronicdisease/about/costs/index.htm . Accessed on June 02, 2024
- Centers for Diseases Control and Prevention. Childhood obesity facts. Available at: https://www.cdc.gov/obesity/data/childhood.html#:~:text=Prevalence%20of%20Childhood%20Obesity%20in%20the%20United%20States&text=The%20prevalence%20of%20obesity%20was,to%2019%2Dyear%2Dolds. Accessed on June 02, 2024
- Orjuela-Grimm, M., Butsch, W.S., Bhatt-Carreño, S. et al. Benchmarking of provider competencies and current training for prevention and management of obesity among family medicine residency programs: a cross-sectional survey. BMC Fam Pract 22, 132 (2021). https://doi.org/10.1186/s12875-021-01484-y
- Amy P. Joseph, Monica Abdelnour, Annelisa Herter, Gerald Miller, Mary Katherine Siebenaler, Janet Patterson; A Quality Improvement Project to Improve the Education Curriculum of a Pediatric Residency Program. Pediatrics February 2022; 149 (1 Meeting Abstracts February 2022): 138.
- Khandalavala B, Koran-Scholl J, Geske J. Comprehensive Obesity Education for Family Medicine. Residents. PRiMER. 2020;4:25. https://doi.org/10.22454/PRiMER.2020.525629