Other Publications
Education Columns
Breastfeeding Education Within a Family Medicine Residency
By Courtney Goettel, MD; Lauren Cooper, MD, UPMC Williamsport Family Medicine Residency, Williamsport, PAIntroduction
While the benefits of breastfeeding are well known, national data continues to show a low rate of breastfeeding continuation. Among the babies born in 2019, 83.2% started out breastfeeding; which reduced to 55.8% receiving some breastmilk and 24.9% being exclusively breastfed at 6 months of age.1 By 12 months, only 35.9% of infants were receiving some breastmilk.1, 2 These numbers have not shown improvement from past years.[2] Family medicine residencies are in a unique position to provide breastfeeding counseling during prenatal, postpartum, and infant continuity visits, which may impact these outcomes. Therefore, educators should ensure residents are equipped with the necessary skills to be successful in this domain. Increased breastfeeding education time has been associated with incorporation of lactation consultants and group prenatal care. Additionally, involvement of lactation consultants is associated with improved perceived resident competence in breastfeeding counseling.3 To address an identified gap within our family medicine residency curriculum, we partnered with a lactation consultant to provide breastfeeding education to our learners.
Methods
We incorporated breastfeeding education delivered by a lactation consultant into our regularly scheduled resident didactics, holding two 1-hour sessions. The lactation consultant was associated with our community-based, academic hospital system and regularly interfaces with our residency program and patient panel. The content included breastfeeding risks and benefits, breastfeeding expectations, and common breastfeeding scenarios. The lactation consultant used demonstration models and identified patient-centered resources. A pre-survey was made available prior to both sessions and a post-survey was administered at the end of the second session. The surveys included questions to assess participant attitudes and knowledge regarding breastfeeding. We compared participant responses between pre and post surveys to assess for any notable differences in participant responses.
Results
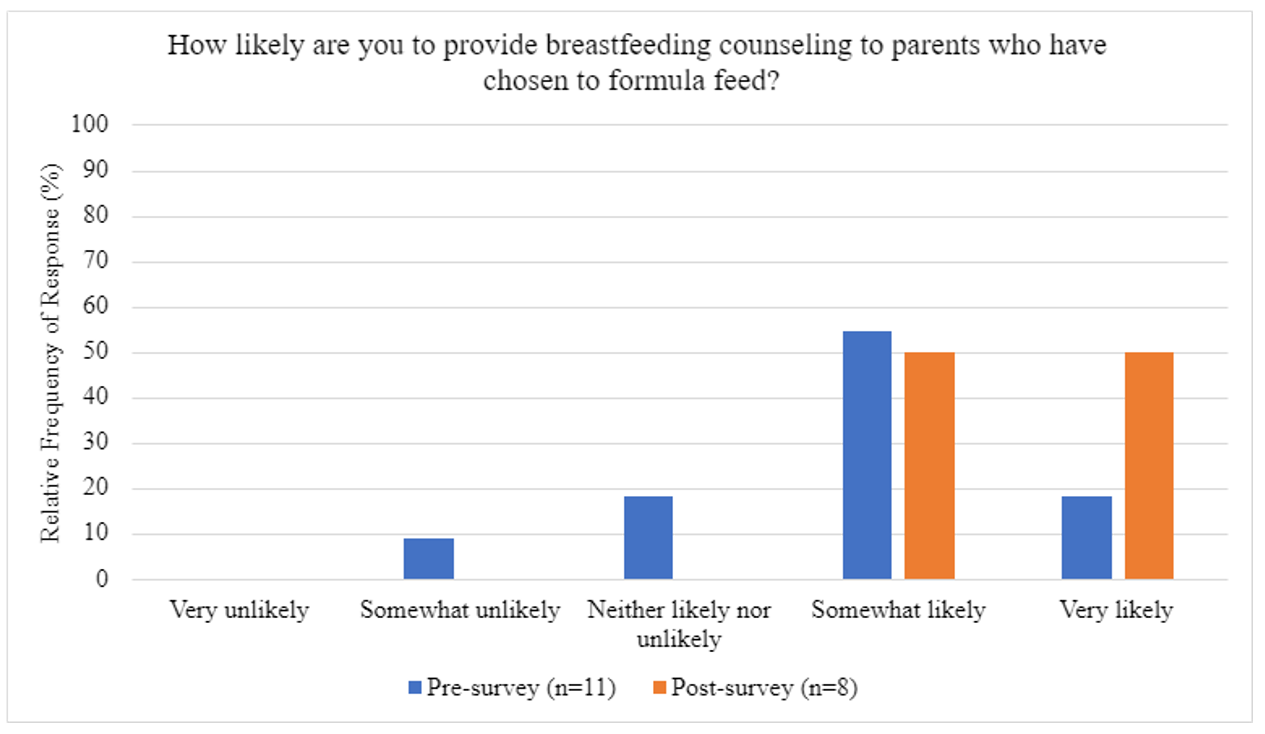
11 attendees completed the pre-survey, and 8 attendees completed the post-survey. Respondents consisted of family medicine residents and faculty. In comparing pre-survey and post-survey data across all respondents, there was an increase in self-reported confidence in educating patients on breastfeeding, likelihood of discussing risks and benefits of breastfeeding during patient visits, and likelihood of providing breastfeeding counseling to parents who have chosen to formula feed (Figures 1-3). Of survey questions related to breastfeeding knowledge, 7 out of 8 were included in analysis of correct responses. Out of these 7 breastfeeding knowledge questions, 2 questions resulted in an improvement in correct responses. The remaining knowledge question was unable to be accurately graded for correctness due to its open-ended format. Respondents consistently demonstrated a positive likelihood of applying didactic material to routine patient care and counseling and an increased interest in learning more about breastfeeding for patient education. On the post-survey, respondents identified new breastfeeding resources learned from the didactic material.
Figures
Figure 1. Confidence with Breastfeeding Patient Education
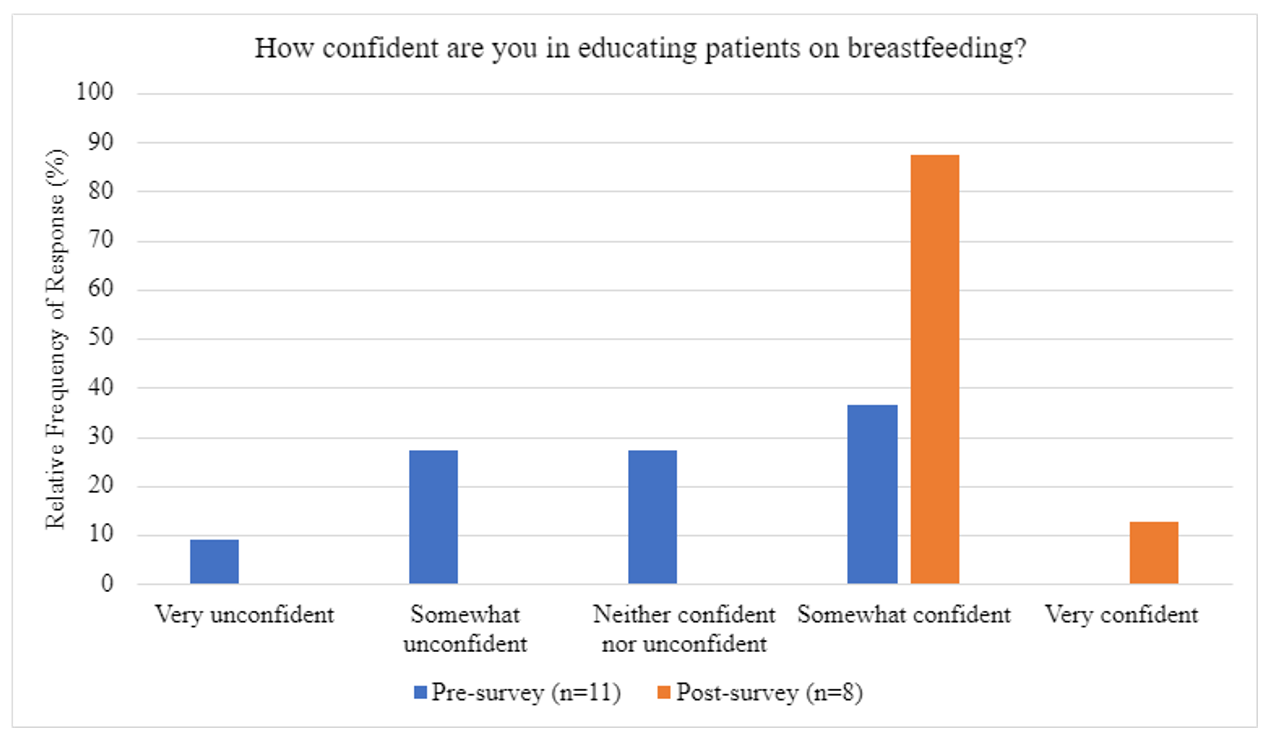
Figure 2. Likelihood of Discussing Breastfeeding Risks and Benefits
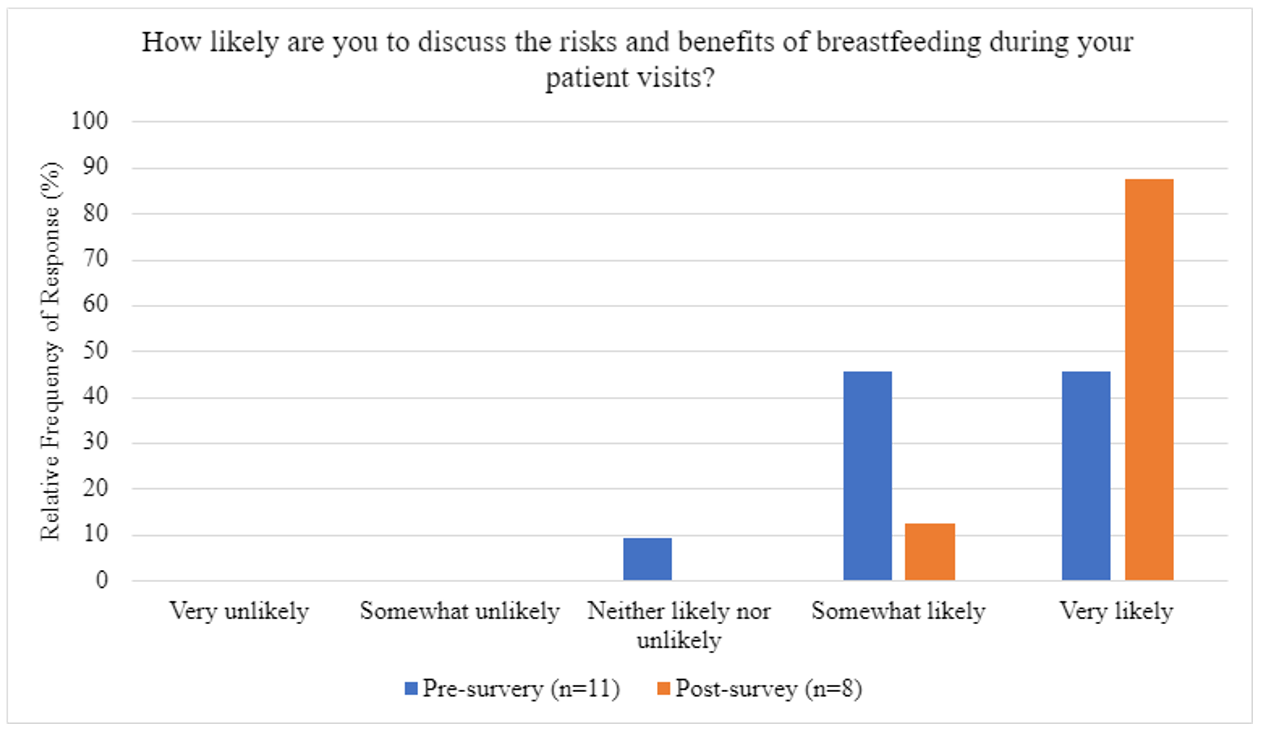
Figure 3. Likelihood of Providing Breastfeeding Counseling to Parents who have chosen Formula Feeding
Discussion
Our study demonstrates that inclusion of breastfeeding didactic materials into a family medicine residency curriculum can improve participant confidence and likelihood of discussing breastfeeding during routine patient care visits. For our residency program, partnering with a lactation consultant within the same hospital system has been an effective approach to expanding the curriculum with no associated extra cost. Following the study, we have expanded our efforts to increase breastfeeding education by starting group patient care visits with the lactation consultant. Next potential steps for our program include restructuring our current breastfeeding curriculum, particularly focusing on knowledge and skill acquisition, analyzing data from breastfeeding group patient visits, and monitoring breastfeeding rates across our patient population in relation to our curriculum.
References
- Centers for Disease Control and Prevention. (2022). Breastfeeding Report Card. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/data/reportcard.htm
- Centers for Disease Control and Prevention. (2023). Results: Breastfeeding Rates. Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/data/nis_data/results.html
- Uzumcu, Z., Sutter, M. B., & Cronholm, P. F. (2020). Breastfeeding Education in Family Medicine Residencies: A 2019 CERA Program Directors Survey. Family Medicine, 52(7), 497–504. https://doi.org/10.22454/FamMed.2020.579473
